Patella Tendinopathy
What is it?
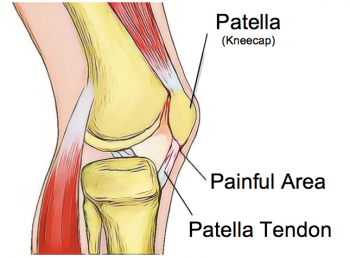
Patella tendinopathy, also known as jumper’s knee, is an overuse disorder characterised by pain at the base of the patella (kneecap) with activities such as squatting, sitting or going up and down stairs. The condition is known as jumpers’ knee because it commonly affects athletes involved in sports that require jumping and repetitive loading of the patella tendon, such as basketball, volleyball, football and tennis.
Landing and jumping activities put a great amount of stress on the patella tendon. This tendon is responsible for transmitting the full force of the quadriceps muscles to the lower leg and during activities such as jumping and landing, this force can actually be many times more than your body weight.
What are the symptoms?
The hallmark sign of patellar tendinopathy is sharp, localised pain in the patellar tendon just below the base of the patella. The pain is usually aggravated by activities that increase load through the quadriceps muscles such as squatting and jumping. Pain associated with patellar tendinopathy usually occurs gradually, often when a person has been very active for a long period of time or if they have recently increased their training schedule. The pain will often start as a small niggle, gradually becoming more noticeable and there may also be a feeling of stiffness with movements of the knee or first thing in the morning.
How does it happen?
Patellar tendinopathy is not a traumatic condition rather, it usually develops gradually over time due to prolonged overloading of the tendon. Like other tissues in the body, tendons are dynamic and can adapt to be able to withstand more force with training. However, if a tendon is unable to adapt to increased load quickly enough, it can develop micro tears leading to pain and dysfunction, known as tendinopathy. The risk of developing this condition can be increased by external factors, such as the type of sports chosen, training volume and the hardness of the training surface.
Intrinsic factors such as bone structure, muscle length, diet, age, muscle strength and overall health can also affect the ability of a tendon to adapt to forces. Anything that impairs the tendon’s ability to absorb force can lead to the development of tendinopathy. In general, men are affected by this condition more often than women.
How can physiotherapy help?
As with all conditions, the first step to effective treatment is an accurate diagnosis. Your physiotherapist will be able to correctly identify this condition and any factors that have led to its development. Treatment for any tendinopathy will involve a degree of rest and reevaluation of your training schedule. Treatment of the tendon itself has been shown to be most effective with a targeted exercise program involving isometric and eccentric muscle contractions. These types of movements have been shown to help stimulate healthy tendon tissue to increase strength and support the damaged tissue, ultimately reducing pain. Tendinopathies can be notoriously difficult to resolve without patience and commitment to a rehabilitation program guided by a physiotherapist.
None of the information in this newsletter is a replacement for proper medical advice. Always see a medical professional for advice on your individual injury.




